Thermometry Learning Module
- Normal body temperature: 36.1-37.5°C (97.0-99.5°F)
- Pyrexia: body temperature above normal
- Low-grade pyrexia: body temperature above normal and up to 38°C (100.4°F)
- Hyperpyrexia: body temperature above 40°C (104°F)
- Fever: abnormal increase in body temperature
- Malignant hyperthermia: rapid rise of body temperature to a dangerous level (41-45°C / 105.8-113.0°F)
- Hypothermia: body temperature <36.1°C (<97°F)
- Core temperature: temperature of the deep internal organs of the body (e.g. liver). The temperature of the skin, fingers, toes can vary within a wide range without performance being impacted but the core body temperature must remain within a very small range to keep the organs’ performance unaffected (36.1-37.5°C / 97.0-99.5°F is generally accepted).
Source: Dougherty and Lister, 2015
Body temperature
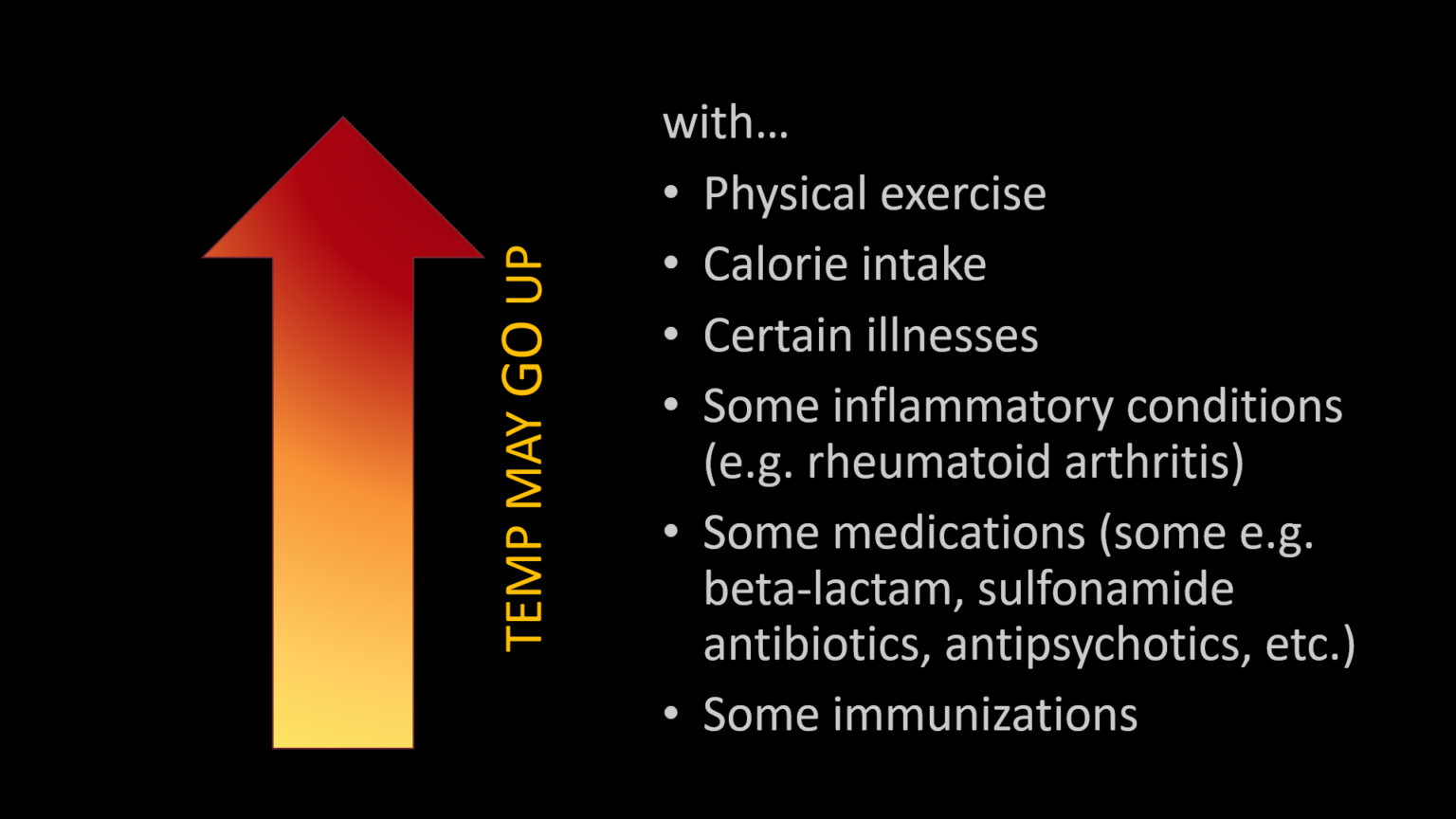
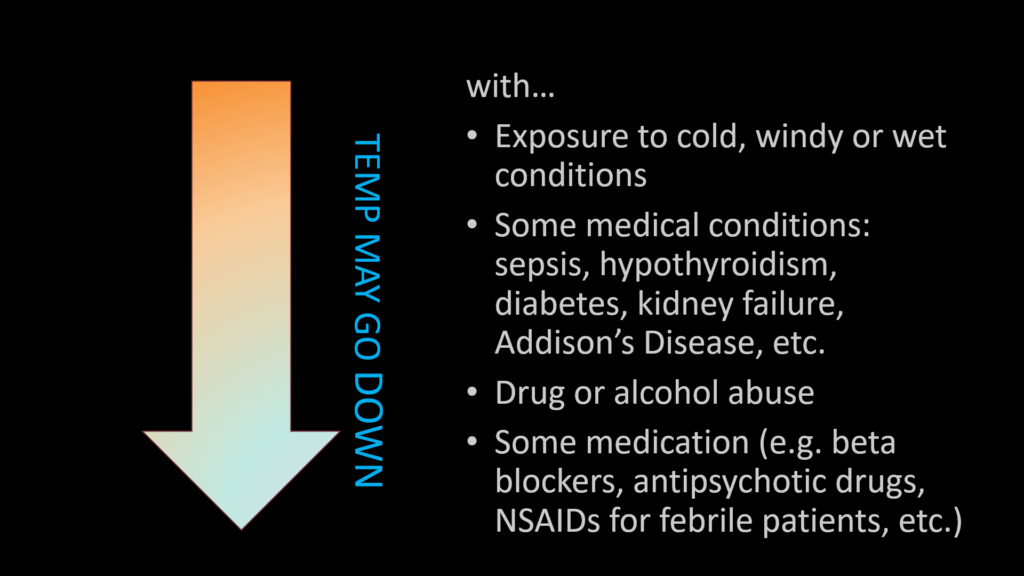
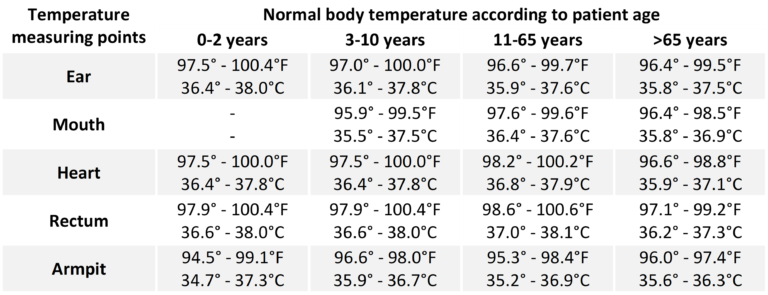
It is a common misconception that 37°C (98.6°F) is the ’normal’ body temperature – it is rather an average value. Normal body temperatures are in a range that varies with age, gender and measuring point, and they vary over the course of the day. It is usually lower in the morning, higher in the afternoon and goes down a little again in the evening. Other factors that affect body temperature include the patient‘s particular activity, metabolic rate or medications taken. Some people may not experience fever even when they are ill. These include, but are not limited to, infants younger than 3 months old, persons with compromised immune systems, persons taking antibiotics, steroids, antipsychotics or antipyretics (aspirin, ibuprofen, acetaminophen), or persons with certain chronic illnesses. The normal body temperature also tends to drop with increasing age.
Normal temperatures are listed in the following table according to the age of the patient and measuring point. Temperatures measured at different parts of the body, even if they are measured at the same time, must not be directly compared with one another as body temperature differs between measuring points.
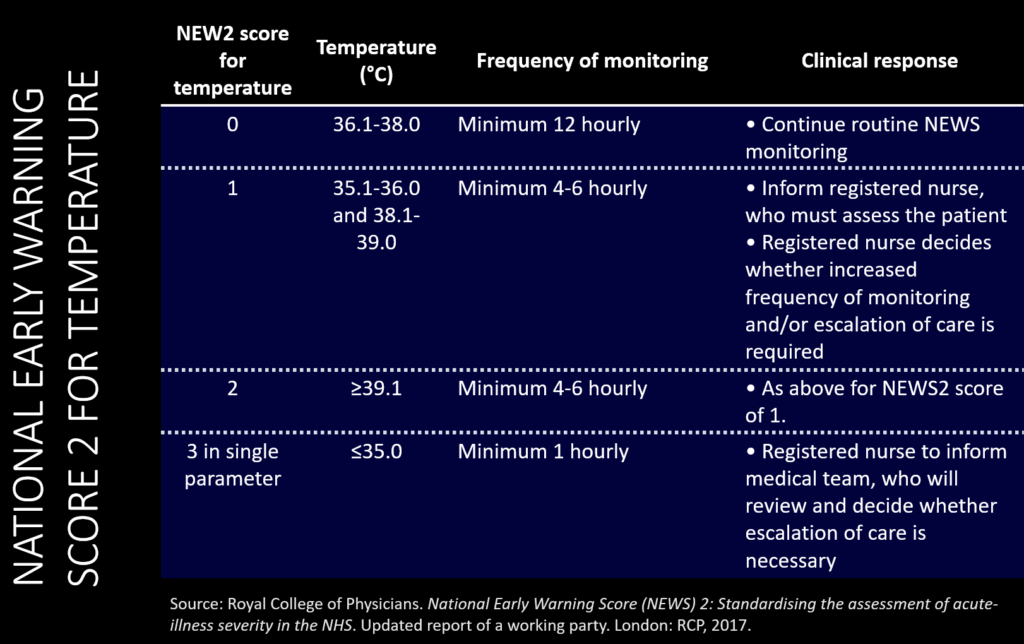
Body temperature is an important component of the National Early Warning Score 2 (NEWS2) and one of the key physiological observations commonly monitored in healthcare settings. It is regulated by the hypothalamus using different physiological mechanisms. When the metabolic activity rises, the body needs to release heat in order to maintain its normal temperature. The most common heat loss mechanism is radiation (heat is transferred from a surface with higher temperature to the surroundings with lower temperature). Other mechanisms include convection (heat is lost through the movement of fluids such as air, e.g. cooling down in front of a fan), conduction (direct heat transfer from a warm surface to a colder surface, e.g. a piece a chocolate that melts when in contact with the hand), and evaporation (e.g. sweating).
The table below should not supersede internal policies and is a simple summary of single-parameter scoring for temperature based on the NEW2 report. Additionally, the report states that “an aggregate score of disturbances in multiple physiological parameters is a more robust measure of acute-illness severity than single-parameter scoring systems.” 1 Finally, “both pyrexia and hypothermia are included in the NEWS, reflecting the fact that the extremes of temperature are sensitive markers of acute-illness severity, sepsis and physiological disturbance.” 1
1 Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: RCP, 2017.
Types of thermometers
- Contact thermometer: oral, tympanic (infrared), temporal (infrared; thermometer often referred to as temporal artery scanner), rectal or axillary measurements
- Non-contact infrared thermometer (NCIT): temporal measurements most common (thermometer often referred to as temporal thermometer or temporal artery thermometer), thermal scanner
- Single-use chemical dot thermometer (note: the UK National Institute for Health and Care Excellence (NICE, 2013) does not recommend the use of forehead chemical thermometers, stating that they are unreliable and should not be used by healthcare professionals.)
-
Invasive thermometer: oesophageal/nasopharyngeal probes, bladder probe, pulmonary artery catheter, etc.
Note: while clinical studies referred to below generally found all but rectal or invasive temperature measurements to be inaccurate, the tympanic and forehead thermometers are still widely used and other studies have found them to be suitable for clinical use. The choice of thermometer should be made based on institutional policies and depending on the risk level and potential severity of the patient’s situation.
A study conducted on children aimed to describe the accuracy to reflect core temperature of a tympanic infrared thermometer, a non-contact infrared forehead thermometer and a temporal artery thermometer (also known as temporal artery scan thermometers) when compared with a rectal thermometer. They found that “all noninvasive techniques underperformed compared with rectal measurement. The temporal artery scan deviations were smallest, but all noninvasive techniques overestimate lower temperatures and underestimate higher temperatures compared with rectal measurement. In our hands, temporal artery scan measurement seems to be second best, but not yet ideal.” (Allegaert et al, 2014). Swedish researchers conducted a systematic review and meta-analysis on the diagnostic accuracy of temporal artery thermometers (TAT) not restricted to age and came to the following conclusion: “TAT is not sufficiently accurate to replace one of the reference methods such as rectal, bladder or more invasive temperature measurement methods. The results are, however, similar to those with tympanic thermometers, both in our metaanalysis and when compared with others. Thus, it seems that TAT could replace tympanic thermometers with the caveat that both methods are inaccurate.” (Geijer et al., 2016).

Contact thermometers require physical contact to operate. A heat sensor is located inside the probe; when in contact with a warmer surface, conduction takes place and the sensor’s temperature rises to that of the warmer surface. There are different types of contact thermometers depending on the type of sensor used: thermocouple, resistance temperature detector (RTD) or thermistor. Thermocouple sensors are cheap and offer a wide temperature range but lack the high level of accuracy needed in healthcare services. Both RTDs and thermistors are found in medical devices and instruments with RTDs being among the most precise temperature sensors available, with measurement uncertainties of ±0.1°C (±0.18°F) or better.
Contact thermometers can be used on the forehead, mouth, armpit or rectum. Accuracy of readings vary between age groups: the gold standard in infants (up to age 3) is rectal measurement but in older age groups, oral measurements generally provide enough accuracy as long as the mouth is kept shut. Axillary (armpit) measurements are the least accurate but may be used in non-acute and low-risk situations where a high level of accuracy is not necessary as they may be better tolerated. Rectal measurements are the most accurate regardless of the age group and should be preferred in acute and high-risk situations.
Because contact thermometers come in contact with the patient, probe covers or proper disinfection are necessary to avoid cross-contamination.
Note: while the tympanic thermometer does come in contact with the ear canal, it does not rely on a heat exchange with a heat sensor (requiring direct contact) to record temperature but rather on the measurement of infrared emissions (which can be done at a distance from a surface). For that reason, it is classified as a non-contact thermometer.

ASTM E1965-98 defines non-contact thermometers, also known as infrared (IR) thermometers, as optoelectronic instruments adapted for non-contact measurement of temperature of a subject by utilizing infrared radiation exchange between the subject and the sensor. They allow for quick readings with the possibility of avoiding direct contact and in some cases, close proximity. ASTM requires an IR thermometer for measuring skin temperature to be accurate to within ± 0.3°C (±0.54°F). For ear canal temperature, the requirement is tighter with ± 0.2°C (±0.36°F). IR thermometers used to measure human body temperature should be approved for clinical use and should offer an adjusted mode which compensates between skin temperature and body core temperature and should allow for calibration with an IR calibrator tool.
Working principle
Every form of matter with a temperature greater than absolute zero (0 K) emits infrared radiation relative to its temperature. This phenomenon is known as characteristic radiation. Different surfaces have different abilities to emit energy by radiation – in other words, they have a different emissivity. By knowing the emissivity of a surface and how much infrared energy it emits, its temperature can usually be determined. Emitted, reflected and transmitted thermal energy from the target is collected onto a lens that pass it on to a detector: the thermopile. A thermopile consists of several thermocouples connected in series and sometimes in parallel; together they convert the thermal energy from the radiation to an electrical signal. Electronic components act as the brain of the thermometer to process the signal to corelate it to the temperature that will ultimately be shown on the display.
Note: Only surface temperatures can be measured by infrared. Environmental conditions involving smoke, dust or steam reduce accuracy.
Appellations
“Clinically validated” means that the device was tested in a clinical trial by an independent party and the results reported were actual, statistically significant and able to pass the strict regulations that pertain to said device. A “clinically validated thermometer” for example would have been validated against international standards thus providing the user with peace of mind knowing that the thermometer is suitable to accurately measure the temperature of all patient populations it is intended for, time and time again. It is a costly process because it is very thorough and must be done by an independent party within a specific set of testing constraints and requirements. Some countries have requirements for periodical verifications to ensure that the required level of accuracy is maintained. For infrared thermometers, this would be done yearly and would require to test the thermometer at 3 different temperatures and to document the results via a test protocol.

“Clinically tested” means that a product was tested in a clinical setting, period. It is much cheaper than clinical validation as the formalities required to validate a product against recognized standards using established protocols are not needed. We don’t know within which set of constraints it was tested and if the results mean anything. No certainty is offered that the unit can be tested again and still provide accurate and reliable results, and no certainty is offered that the unit can be calibrated once out of the factory.
“Clinically studied” means that someone looked at a product in a clinical setting. We don’t know that if we test it, it will produce accurate and reliable results, and we don’t know that we can calibrate it so that it keeps producing accurate and reliable results over its lifetime, if it did in the first place. This is the cheapest, and most deceptive way to get in the word “clinical” without needing to reveal results.
Coronavirus disease 2019 (COVID-19) – Symptoms, diagnosis and treatment | BMJ Best Practice
Dante A, Franconi I, Marucci AR, Alfes CM, Lancia L. Evaluating the Interchangeability of Forehead, Tympanic, and Axillary Thermometers in Italian Paediatric Clinical Settings: Results of a Multicentre Observational Study. J Pediatr Nurs. 2020 May-Jun;52:e21-e25. doi: 10.1016/j.pedn.2019.11.014. Epub 2019 Dec 14. PMID: 31848034.
Dougherty L, Lister S (2015) The Royal Marsden Manual of Clinical Nursing Procedures. Wiley-Blackwell.
Geijer H, Udumyan R, Lohse G, et alTemperature measurements with a temporal scanner: systematic review and meta-analysisBMJ Open 2016;6:e009509. doi: 10.1136/bmjopen-2015-009509.
Karel Allegaert, Kristina Casteels, Ilse van Gorp, Guy Bogaert, Tympanic, Infrared Skin, and Temporal Artery Scan Thermometers Compared with Rectal Measurement in Children: A Real-Life Assessment, Current Therapeutic Research, Volume 76,2014, Pages 34-38, ISSN 0011-393X, doi: 10.1016/j.curtheres.2013.11.005.
Heat Convection – an overview | ScienceDirect Topics
Infrared Emissivity Table | ThermoWorks
Measuring body temperature using a tympanic thermometer | Nursing Times
National Early Warning Score (NEWS) 2 | RCP London
Thermometers: Understand the options – Mayo Clinic